|
|
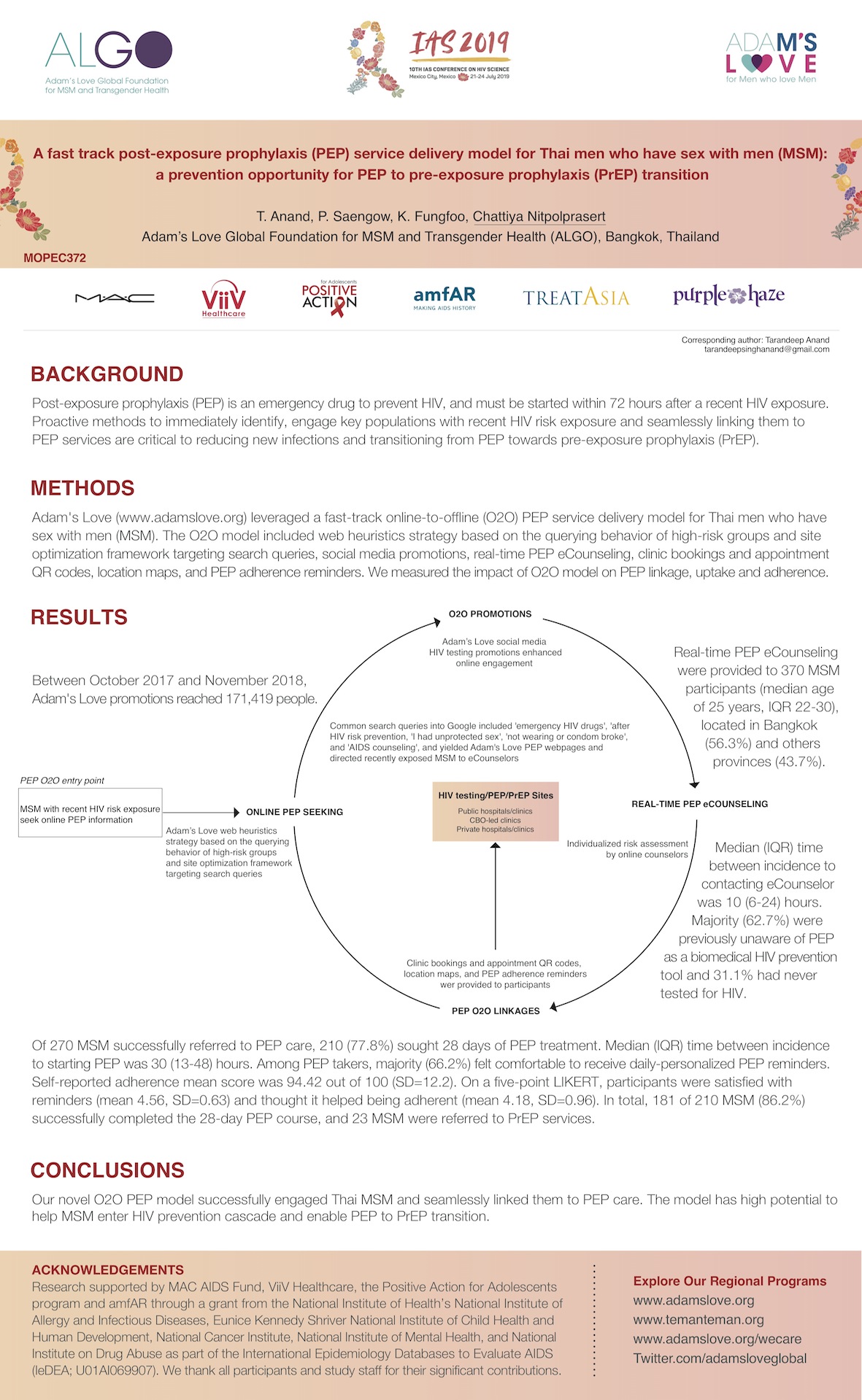
A fast track post-exposure prophylaxis (PEP) service delivery model for Thai men who have sex with men (MSM): A prevention opportunity for PEP to pre-exposure prophylaxis (PrEP) transition Title A fast track post-exposure prophylaxis (PEP) service delivery model for Thai men who have sex with men (MSM): A prevention opportunity for PEP to pre-exposure prophylaxis (PrEP) transition http://programme.ias2019.org/Abstract/Abstract/449 Download the e-Poster https://programme.ias2019.org//PAGMaterial/eposters/449.pdf Conference 10th IAS Conference on HIV Science | 21-24 July 2019 | Mexico City, Mexico Presenter Chattiya Nitpolprasert Background: Post-exposure prophylaxis (PEP) is an emergency drug to prevent HIV, and must be started within 72 hours after a recent HIV exposure. Proactive methods to immediately identify, engage key populations with recent HIV risk exposure and seamlessly linking them to PEP services are critical to reducing new infections and transitioning from PEP towards pre-exposure prophylaxis (PrEP). Methods: Adam''s Love (www.adamslove.org) leveraged a fast-track online-to-offline (O2O) PEP service delivery model for Thai men who have sex with men (MSM). The O2O model included web heuristics strategy based on the querying behavior of high-risk groups and site optimization framework targeting search queries, social media promotions, real-time PEP eCounseling, clinic bookings and appointment QR codes, location maps, and PEP adherence reminders. We measured the impact of O2O model on PEP linkage, uptake and adherence. Results: Between October 2017 and November 2018, Adam''s Love promotions reached 171,419 people, and real-time PEP eCounseling were provided to 370 MSM participants (median age of 25 years, IQR 22-30), located in Bangkok (56.3%) and others provinces (43.7%). Median (IQR) time between incidence to contacting eCounselor was 10 (6-24) hours. Common search queries into Google included ''emergency HIV drugs'', ''after HIV risk prevention, ''I had unprotected sex'', ''not wearing or condom broke'', and ''AIDS counseling''. Majority (62.7%) were previously unaware of PEP as a biomedical HIV prevention tool and 31.1% had never tested for HIV. Of 270 MSM successfully referred to PEP care, 210 (77.8%) sought 28 days of PEP treatment. Median (IQR) time between incidence to starting PEP was 30 (13-48) hours. Among PEP takers, majority (66.2%) felt comfortable to receive daily-personalized PEP reminders. Self-reported adherence mean score was 94.42 out of 100 (SD=12.2). On a five-point LIKERT, participants were satisfied with reminders (mean 4.56, SD=0.63) and thought it helped being adherent (mean 4.18, SD=0.96). In total, 181 of 210 MSM (86.2%) successfully completed the 28-day PEP course, and 23 MSM were referred to PrEP services. Conclusions: Our novel O2O PEP model successfully engaged Thai MSM and seamlessly linked them to PEP care. The model has high potential to help MSM enter HIV prevention cascade and enable PEP to PrEP transition. |