|
|
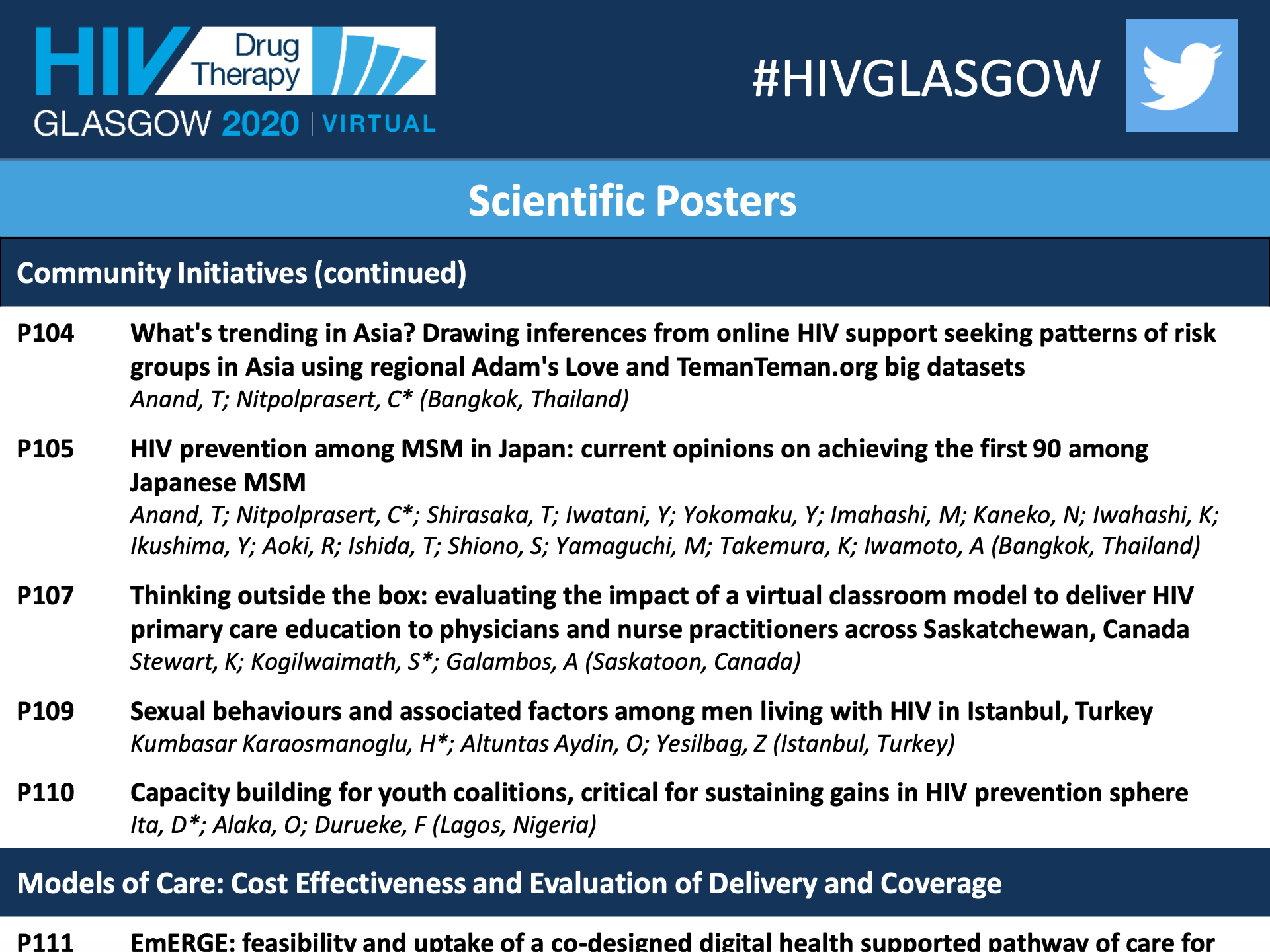
HIV PREVENTION AMONG MSM IN JAPAN: CURRENT OPINIONS ON ACHIEVING THE FIRST 90 AMONG JAPANESE MSM
HIV PREVENTION AMONG MSM IN JAPAN: CURRENT OPINIONS ON ACHIEVING THE FIRST 90 AMONG JAPANESE MSM
HIV Drug Therapy Glasgow 2020 – Virtual, 5–8 October 2020
Journal of the International AIDS Society ( IF 5.553 ) Pub Date : 2020-10-05 , DOI: 10.1002/jia2.25616
Watch video presentation at Conference website https://vimeo.com/464496985 Download Adam's Love Japan Research published online via the Journal of the International AIDS Society. Abstracts. Open Access. HIV Glasgow – Virtual, 5–8 October 2020. P105
HIV prevention among MSM in Japan: current opinions on achieving the first 90 among Japanese MSM
Tarandeep Anand1; Chattiya Nitpolprasert1; Takuma Shirasaka2; Yasumasa Iwatani3; Yoshiyuki Yokomaku3; Mayumi Imahashi3; Noriyo Kaneko4; Kota Iwahashi5; Yuzuru Ikushima6; Rieko Aoki7; Toshihiko Ishida8; Satoshi Shiono9; Masazumi Yamaguchi10; Keizo Takemura11 and Aikichi Iwamoto12
1Adam's Love Global Foundation for MSM and Transgender Health ALGO, HIV Prevention, Bangkok, Thailand. 2National Hospital Organization Osaka National Hospital, AIDS Medical Center, Osaka, Japan. 3Clinical Research Center, National Hospital Organization Nagoya Medical Center, Department of Infectious Diseases and Immunology, Nagoya, Japan. 4Nagoya City University, Graduate School of Nursing, Nagoya, Japan. 5AKTA, Community Center, Tokyo, Japan. 6Positive Living and Community Empowerment TOKYO, Tokyo, Japan. 7Center for Health and Rights for Migrants, Osaka, Japan. 8Rise, Community Center, Nagoya, Japan. 9Dista, Community Center, Osaka, Japan. 10Bunan Hospital, Department of Internal Medicine, Kawaguchi, Japan. 11The Sumitomo Foundation, Tokyo, Japan. 12Japan Agency for Medical Research and Development AMED, Department of Research Promotion, Tokyo, Japan Background: Japan is a developed nation with an HIV epidemic concentrated among MSM [1]. Despite success in exceeding the second and third UNAIDS 90‐90‐90 targets, Japan has lagged behind on first 90. Approximately 30% of newly reported cases have been annually identified by AIDS onset [2], implying reaching subpopulations for early HIV testing remains primary challenge.
Methods: In 2019, interviews were conducted with medical professionals at AIDS Core Hospitals (serving >6000 HIV‐positive people), HIV researchers, governmental agencies and community staffs in Tokyo, Nagoya, Kanagawa and Osaka. We sought to understand current HIV testing alternatives, reasons behind late diagnosis, and identified immediate strategies for scaling‐up early HIV testing.
Results: Municipal healthcare centres remain key sites delivering free/anonymous HIV/STI testing, although their women/child health focus limits uptake among MSM. Primary reasons for late HIV diagnosis included challenges in reaching and engaging MSM in HIV cascades, structural barriers i.e. testing capacity, schedule/accessibility, lack of MSM‐friendly services and regulatory issues with HIV self‐testing. In Japan, community organisations are spearheading HIV testing initiatives by implementing prefecture‐based models. For example, HIVCheck.jp Tokyo, an HIV self‐testing research piloted in collaboration with clinical laboratory led to increased HIV testing uptake among MSM (1127 DBS samples collected), with provisional positive rate of 2.4% [3]. In Nagoya, HIV testing during 2018 LGBT event has seen two‐fold year‐on‐year increase in HIV testing (approx. 700 MSM). In Osaka, bimonthly, weekend‐based HIV/STI testing programme (engaging 30 to 40 MSM) offers low‐cost HIV testing during late hours at collaborated private clinics. Japanese MSM actively use internet for seeking sex partners, e.g. gay dating app 9monsters has reportedly >300 000 active members. While traditional outreach approaches at gay hotspots are widely prevalent, sexual health campaigns (e.g. Sailor Moon) to stem rapid rise of STI cases by government has had limited impact among MSM.
Conclusions: To reach the first 90, Japan needs diffusion of innovative technology to streamline its HIV service delivery and develop a culturally sensitive communications strategy. To ensure seamless virtual to critical offline HIV services transition, Japan should implement an integrated Online‐to‐Offline (O2O) model offering real‐time eCounselling and online bookings (QR codes) to ensure privacy and real‐time monitoring features to help track/validate participants [4,5].
References:
1. Iwamoto A, Taira R, Yokomaku Y, Koibuchi T, Rahman M, Izumi Y, et al. The HIV care cascade: Japanese perspectives. PLoS One. 2017;12:e0174360.
2. Matsuoka S, Nagashima M, Sadamasu K, Mori H, Kawahata T, Zaitsu S, et al. Estimating HIV‐1 incidence in Japan from the proportion of recent infections. Prev Med Rep. 2019;16:100994.
3. Iwahashi K. Dried blood spot based HIV testing ‘HIVcheck.jp’ is a new testing opportunity for men who have sex with men in Tokyo, Japan [oral abstract]. Fast‐Track Cities 2019; 2019 Sep 8‐11; London, United Kingdom; 2019.
4. Anand T, Nitpolprasert C, Trachunthong D, Kerr SJ, Janyam S, Linjongrat D, et al. A novel Online‐to‐Offline (O2O) model for pre‐exposure prophylaxis and HIV testing scale up. J Int AIDS Soc. 2017;20:21326.
5. Anand T, Nitpolprasert C, Phanuphak N. Online‐to‐Offline (O2O) models in HIV service delivery. Curr Opin HIV AIDS. 2017;12:447‐57.
|